North Carolina Cancer Prevention and Control Branch
North Carolina Comprehensive Cancer Control Program
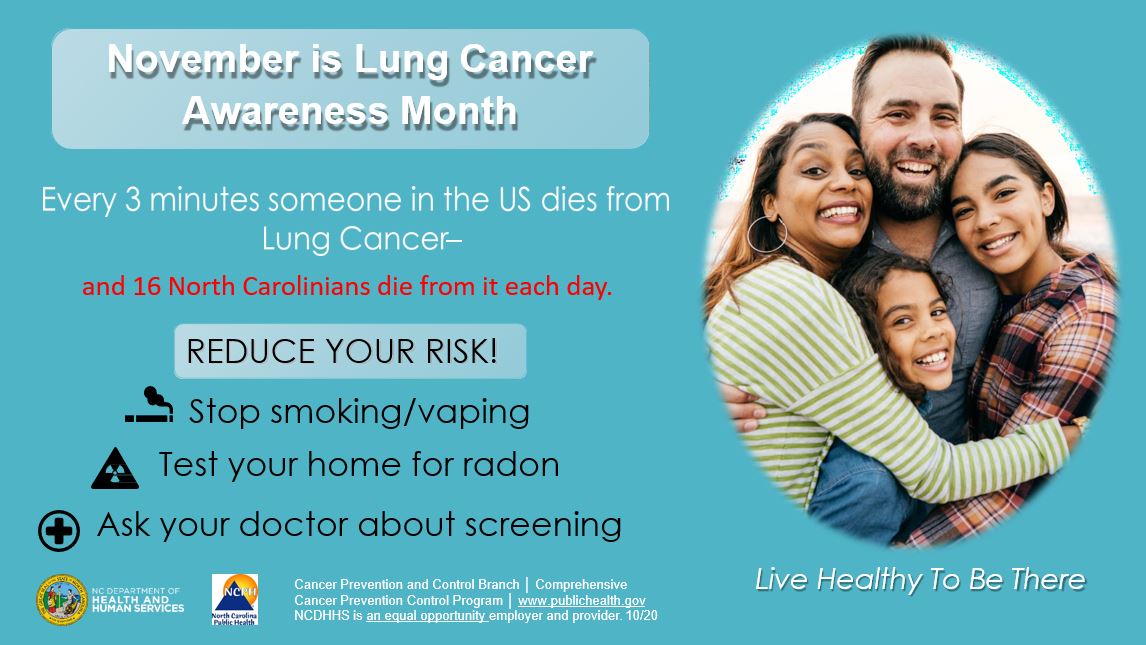
Lung Cancer

Lung Cancer Health Promotion


CDC: TIPS From Formers Smokers - Brian H. - Do You Know?
La historia de Brian H. | Historias de la vida real | Consejos de exfumadores | CDC
Eddie's Story: Test. Fix. Save a Life – YouTube Video
In Eddie's Story, the winner of EPA's 2008 "Test. Fix. Save a Life." video contest, lung cancer survivor Eddie Metcalfe shares his personal story - a powerful call to action for every American home to be tested for radon. Share with your friends, and please have your home tested.

What is Lung Cancer?
Refers to any cancer that forms in the tissues of the bronchus or lung. Lung cancers are usually grouped in two main types, small cell and non-small cell. These differ in how fast they grow and how they are treated. Non-small cell lung cancer is more common than small cell lung cancer. Smoking is a major risk factor for both types of lung cancer. Approximately 80% of all lung cancer is caused by cigarette smoking.1 Among people who have never smoked, radon is the leading cause of lung cancer. People who smoke and are exposed to radon have an increased risk of lung cancer.2
Symptoms
Most people do not have any symptoms of lung cancer until the cancer is advanced. Lung cancer symptoms may include:
- coughing that gets worse or does not go away,
- chest pain,
- shortness of breath,
- wheezing,
- coughing up blood,
- feeling very tired all time and/or
- unexplained weight loss.3

Screening
Screening with low-dose spiral computed tomography (LDCT) can reduce lung cancer deaths by about 20% compared to standard chest x-ray among current or former heavy smokers.
Lung cancer screening is recommended if you are someone who:
- is between 50 and 80 years old.
- has a 20 pack-year history. This means patients will be eligible if they, for example, smoke one pack a day for 20 years or two packs a day for 10 years and
- currently smoke or have quit within the past 15 years.
Talk to your doctor about getting a lung cancer screening.

Treatment
Treatment is usually most successful when cancer is detected early. Lung cancer treatment options include surgery, chemotherapy, radiation and targeted cancer therapies. Small cell and non-small cell lung cancers are treated in different ways. Talk to your cancer doctor about the treatment options available for your type and stage of cancer. Your doctor can explain the risks and benefits of each treatment and their side effects. 6

Risk Factors
These risk factors may increase your chances for developing lung cancer.
- Tobacco use (cigarette, cigars, pipe, e-cigarettes, vape pens and e-hookah).
- Exposure to environmental hazards (secondhand smoke, radon, asbestos, coal dust, other chemicals or substances).
- Radiation therapy to the chest.
- Personal and/or family history of lung cancer.
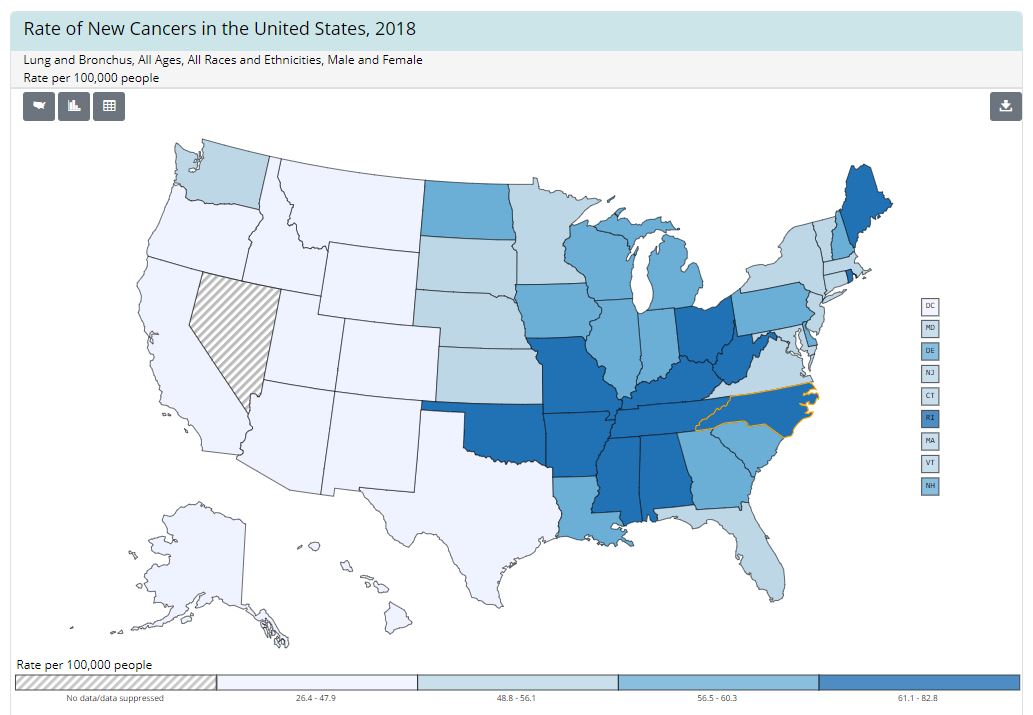
Lung Cancer in NC
Lung cancer was the leading cause of cancer deaths in North Carolina in 2020 (5,019 deaths). It is estimated that 9,247 people in North Carolina will be diagnosed with lung cancer and 5,671 people will die from lung cancer in 2022. Since 2000, the rates of new lung cancer cases and lung cancer deaths have decreased in North Carolina. However, the North Carolina rates are still higher than the national rates.4






- Quit tobacco and vaping use. Quitting takes practice! Coaching and medications can triple your chances of quitting for good. Call 1-800-Quit-Now or check out QuitlineNC.com for help.
- Avoid exposure to secondhand smoke.
- Test your home for radon. Radon is a gas that can be in the soil and ground water. Homes in all 100 counties have tested at high levels for radon. The only way to know if your home has a radon problem is to test it .For testing well water, contact the environmental health program at your local health department. For testing air, contact 919-814-2290 or http://www.ncradon.org/Testing.html.
- Be aware of workplace environmental hazards. Avoid exposure to cancer-causing chemicals or substances. Follow safety procedures.
- Get a lung cancer screening, if eligible.
- Know your family health history including cancer illnesses and deaths.
- Eat Healthy. Eat more fruits and vegetables, drink more water and fewer sugar-sweetened beverages and create meal plans to cook at home.
- Be physically active. Strive to get at least 30 minutes of physical activity 5 days a week and strength training at least twice a week.
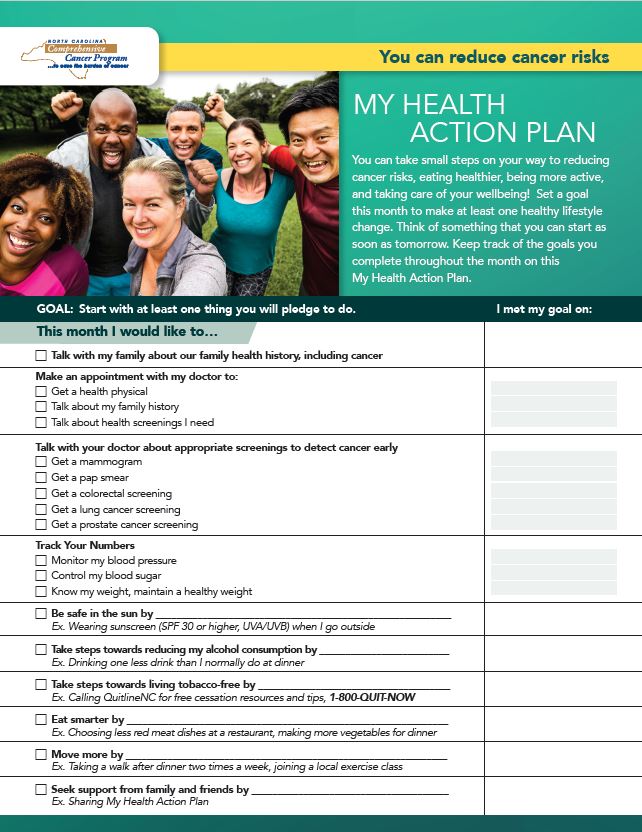
Take action!
Use My Health Action Plan to set monthly goals to make healthy lifestyle changes.
Don’t wait. Start on your My Health Action Plan today!
A Cancer Diagnosis is an Unexpected Journey
Talk with your healthcare provider about a health care plan to help track your care and to support your physical and emotional health needs. Ask for a patient navigator. They will help guide you through your journey and connect you to resources and support services. Be your own advocate. Build your support circle. Continue to take steps to be healthy. These steps may help improve your quality of life and lower the risk of your cancer returning.
Checking into a better me: The how-to guide for optimal health for women.
Use this journal guide to record and track important information about your health history, current medicines, health care providers, appointments, treatments, health numbers, health tips, and screenings all in a convenient checkbook.
Take this guide with you to your check- ups to have the information you might need during your visit, to track your personal health action plan and your healthy living journey. There is space for you to record questions and answers and to take notes.
Way to Play: Men's Health Playbook
Use this Men’s Health Playbook to keep your body running its best. This tool is designed for men ages 18-45 years. Use it to record your medical history and routine plays. Map out your health goals as you move toward a healthier you!
Be sure to keep your playbook with your other important papers or where you can’t forget it for your next health team meetup.
Need help? Talk to your healthcare provider or visit the resources below.
- American Cancer Society
- Centers for Disease Control and Prevention, Lung Cancer Screening.
- Lung Cancer Initiative of North Carolina.
- NC DHHS, Cancer Prevention and Control Branch.
- NC Radon Program.
- NC Tobacco Prevention and Control Branch.
- NCCARE360
Additional Resources
Visit the Hub NC Comprehensive Cancer Control Program Resource Hub to view all additional resources. Below are a few for quick access.
Cancer Branch Information
- Breast Cancer
- Cancer Branch Home Page
- Caregiving
- Cervical Cancer
- Colorectal Cancer
- Contact Us
- COVID-19 Resources
- Data
- Health Equity
- Lung Cancer
- NC Advisory Committee on Cancer Coordination and Control
- NC Breast and Cervical Cancer Control Program
- NC Comprehensive Cancer Control Program
- NC Comprehensive Cancer Control Program Resource Hub
- NC WISEWOMAN Project
- Online Resources
- Proste Cancer
- Skin Cancer
- Survivorship
- Treatment
Last Modified: 11-08-2022



 Lung Cancer Fact Sheet
Lung Cancer Fact Sheet
 NC Cancer Plan 2020-2025
NC Cancer Plan 2020-2025
 Reducing the Burden of Cancer
Reducing the Burden of Cancer
 Lung Cancer Awareness Month Social Media Toolkit
Lung Cancer Awareness Month Social Media Toolkit